Advance Surgical - Bariatric surgeon Perth
Battling
your
weight?
Our integrated team of bariatric surgeons and physicians, dietitians and psychologists are here to assist your throughout your weight loss journey.
Check if you are a candidate for bariatric surgery.
Queries will be answered by Dr Jon Armstrong.

Bariatric Surgeon perth
Results from real people
Natasha had a gastric sleeve in May 2018. Fast forward to March 2019; Natasha lost 35kg and is 20 weeks pregnant.

Bariatric Surgeon perth
Results from real people
Lost 43 kg since 2016. Now at 55 kg, Beata exercises regularly and gets full support from her family and friends.

Bariatric Surgeon perth
Results from real people
11 months since weight loss surgery and lost 40 kgs. Went from 3XL to a M. Mark is very organised with healthy food choices.

Bariatric Surgeon perth
Results from real people
Kristen had a gastric sleeve and lost 50kg since.
Weight loss surgeon Perth
Weight
loss
surgeries
Understanding the different types of weight loss procedures (also called bariatric surgery) available at Advance Surgical, in Perth.
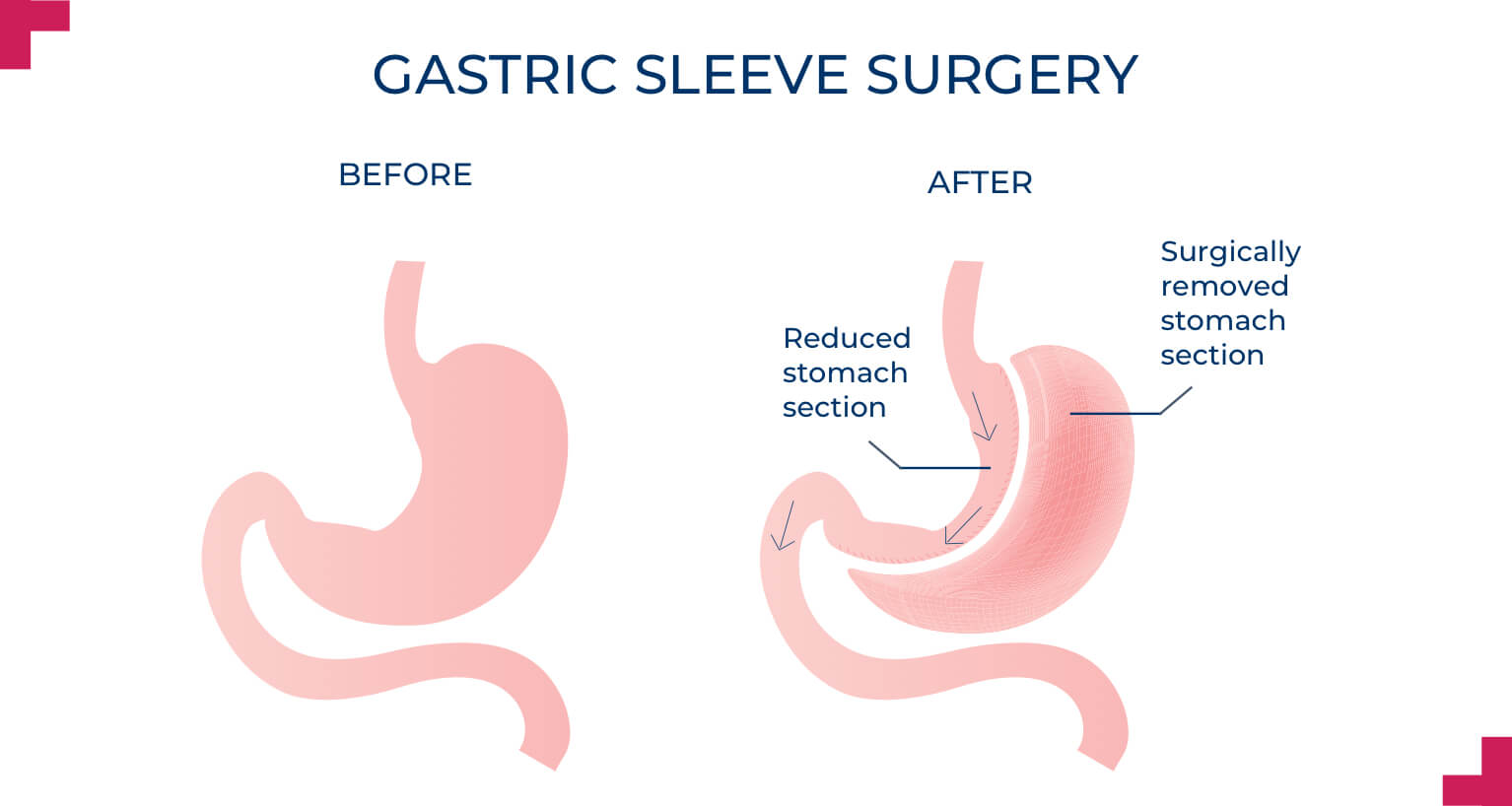
Gastric sleeve surgery
What is gastric sleeve surgery, explained by Perth bariatric surgeon Mr Jon Armstrong
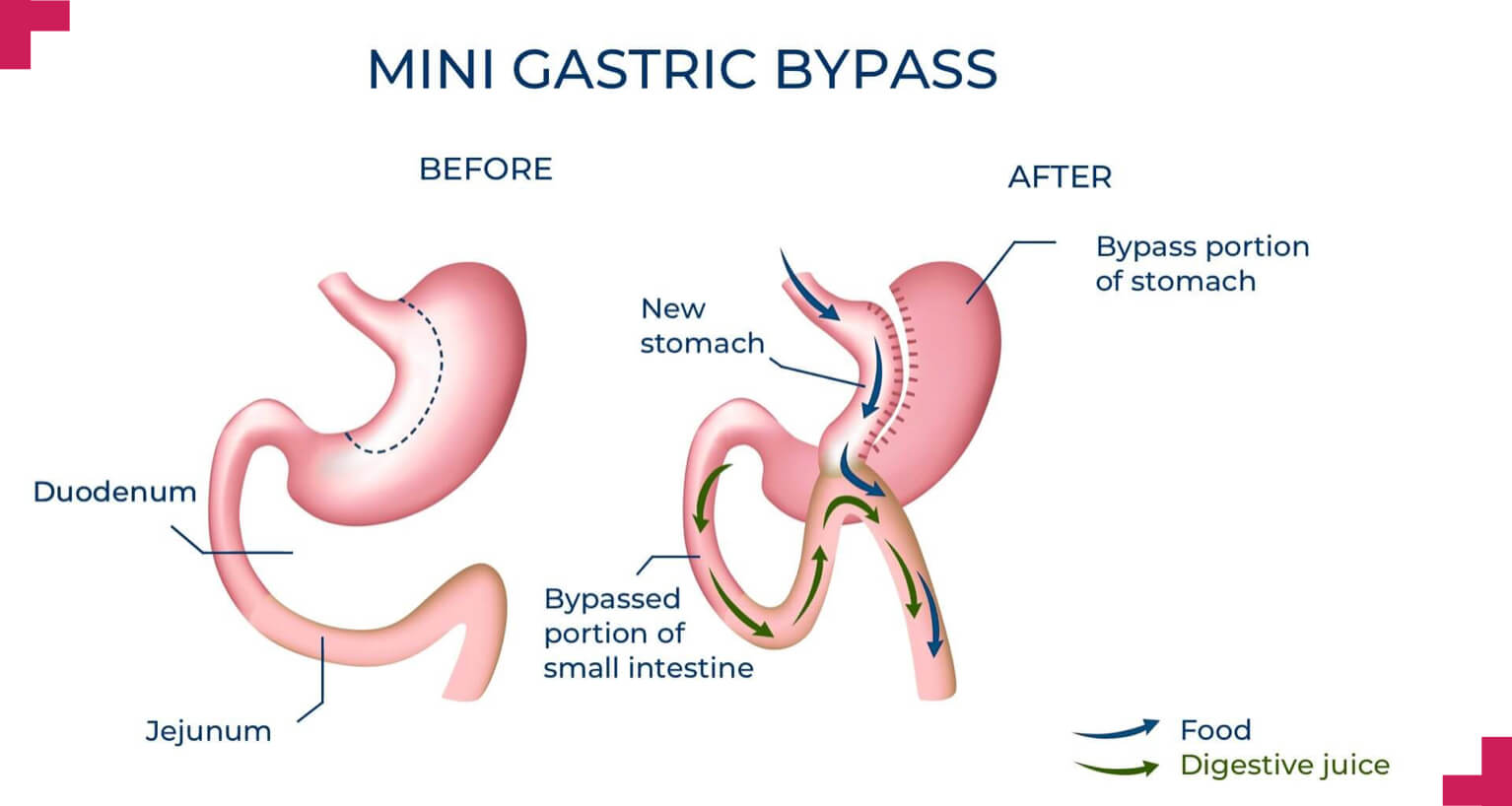
Mini-gastric bypass surgery
What is a mini-gastric bypass, explained by Perth bariatric surgeon Mr Jon Armstrong
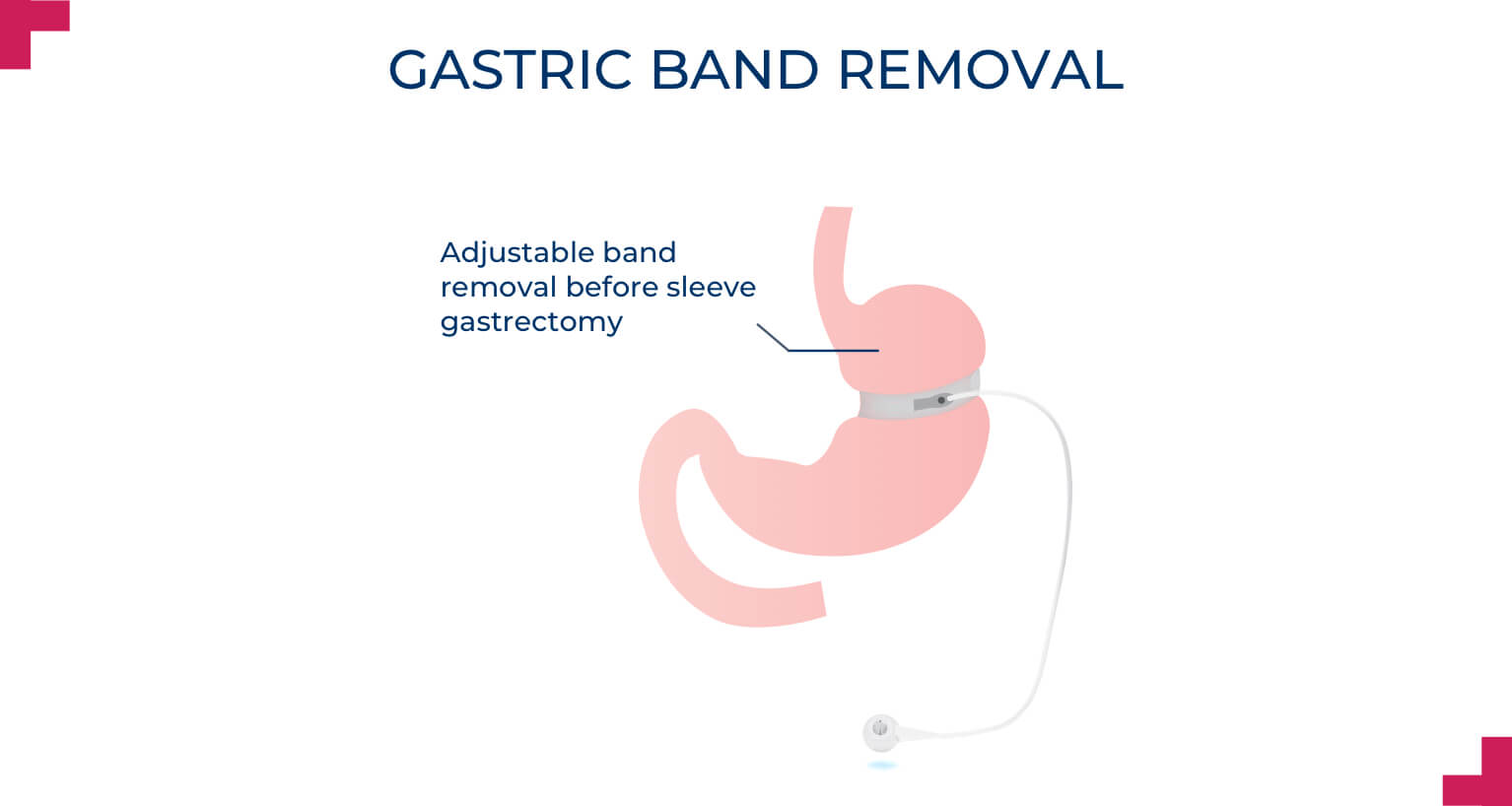
Gastric band removal
Can I have gastric sleeve surgery after I have a gastric band removed?
At Advance Surgical, Mr Jon Armstrong and the team help people who want to lose weight through bariatric surgery.
Bariatric surgeon Perth
About
Advance
Surgical
Established in 2005
When we established Advance Surgical our motivation was to help those who find that diet and exercise are simply not working for them.
The cost of bariatric surgery
We understand the cost of bariatric surgery may be an issue. We have changed our pricing to be more affordable. Payment plans available.
Team of specialists
Mr Jon Armstrong, Medical Director and Founder alongside the team at Advance Surgical, have helped thousands of people in Perth.
How bariatric surgery can help you
You are not
alone!
1 in 3 adult
Australians
is obese
When you have a BMI over 35 you’re at a higher risk of developing type 2 diabetes, high blood pressure, heart disease, cancer, fertility problems, sleep apnoea, and arthritis and joint issues.
If you believe you have medical reasons for weight loss surgery, please get in touch with our friendly team at Advance Surgical.

Medical reasons for bariatric surgery
What are the real medical reasons for weight loss surgery? Perth bariatric surgeon Dr Jon Armstrong explains.

Are you a candidate for bariatric surgery?
Check if you are eligible. Queries will be answered by our bariatric surgeon Dr Jon Armstrong.
Check if you are a candidate for bariatric surgery.
Queries will be answered by Dr Jon Armstrong.